OVdialogue – consider joining our team in the role of Peer Support Volunteer. Over a few hours each week, you would be part of a team that helps connect people, support conversations and are thought leaders for OVdialogue. This is your opportunity to give back to those who have/continue to support you through the tough times, share your unique experiences, and help celebrate successes. For more details of what this entails, please reach out to @Mfallis (mfallis@ovariancanada.org).
Does anyone know if Cytalux during surgery is available in Canada?
Comments
-
I don't believe it's been approved in Canada, however there appears to be work underway here , eiher on it or a similar tool. One of our Personal Support Volunteers sent lme this article about a week ago.
Team working toward first-in-human trial of new theranostic tool win Beyond Chemotherapy Grand Challenge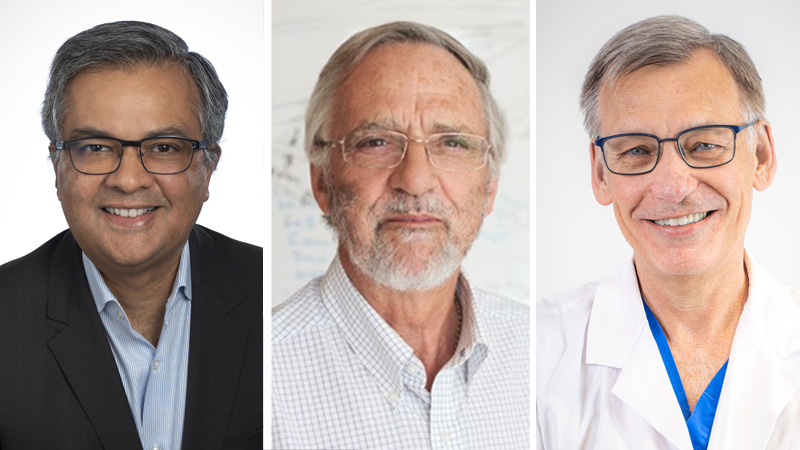
Drs. Amit Oza, Brian Wilson and Jonathan Irish will use the $500,000 award to help finance a safety trial using the new method of identifying tumours in real-time in the operating room. (Photos: UHN)A group of UHN clinicians and scientists testing a new way to pinpoint cancerous tumours have won the first Agnico Eagle Grand Challenge "Beyond Chemotherapy" Award.
The Princess Margaret Cancer Centre group led by Drs. Amit Oza, Jonathan Irish and Brian Wilson will use the $500,000 award to help finance a world's first-in-human safety trial using the new method of identifying tumours in real-time in the operating room.
"We're going to start with patients with gynecologic cancer," says Dr. Oza, a medical oncologist. "As soon as we show proof of principle that this is safe and tolerable, we will then be leveraging it into studies in head and neck cancer, lung cancer, prostate cancer and other specific gynecological cancers."
The diagnostic tool at the centre of the group's "proof of principle" is called porphysomes, an organic nanoparticle that lights up red when exposed to blue. It was discovered in 2011 by Princess Margaret Senior Scientist Dr. Gang Zheng. Since then, Dr. Zheng and colleagues have put porphysomes through numerous rigorous pre-clinical trials.
"You may consider porphysomes as like a 'homing beacon,'" explains Dr. Zheng. "It will help a surgeon more easily identify and localize the tumour and distinguish it from surrounding normal tissues.
"That will help the surgeon resect the tumour more completely and in a minimally-invasive way."
The advance here is significant because around 20 percent of patients with invasive cancer can have cancer remaining after surgery, despite the best clinical practice. That means the patient has to come back for another operation.
The porphysome-enabled fluorescence image-guided surgery increases the precision of disease resection, enables clearer surgical margins, and aids in the complete resection of metastatic deposits and malignant lymph nodes. This increased surgical precision with intraoperative imaging can also reduce disease recurrence and improve disease-free survival.
Potential 'game-changer in oral cancer'
Dr. Irish is the lead for the surgical teams that include gynecological, head and neck, thoracic and prostate surgical oncologists who will be testing the accuracy of porphysomes to light up a tumour in patients. If successful, he sees this first porphysome trial as a gateway to broader clinical applications.
"I think it has high potential to be a game-changer in oral cancer," says Dr. Irish, "and in other areas like advanced endometrial cancer and lung cancer, where porphysomes will enable the detection of regional disease and allow the surgeon to follow the spread of the cancer lymphatically."
Preparation for this world-first-in-human trial is in the final phase of Research Ethics Board and Health Canada regulatory approval. The trial will be based at the Princess Margaret Cancer Centre and Toronto General Hospital, with 20 to 30 patients to be enrolled. The porphysome nanoparticles will be administered by intravenous injection and delivered via a fatty lipid that acts as a protective covering – the same delivery vehicle as the mRNA vaccine for COVID-19.
The Princess Margaret group is eager to determine safety because of the additional benefits of porphysomes, which Dr. Zheng likens to a Swiss Army Knife. Porphysomes are not only a superior diagnostic imaging tool – the "homing beacon" – but can also be used as a light-based therapy with the potential for drug delivery.
The "Beyond Chemotherapy" potential of this program is to combine diagnosis and therapeutic approaches for cancer, an approach also known as theranostics.
An example of the power of theranostics can be appreciated by other qualities of the porphysome molecule. When exposed to higher intensity light, porphysomes absorb the energy and heat the tissue locally to shrink and eliminate cancerous tissue, thereby becoming "a killer beacon."
"The elegance here is that we can use light to activate the porphysomes to provide other photodynamic or photothermal treatments for minimally-invasive destruction of the tumour," says Dr. Wilson, a biophysicist. "The unique multifunctionality of porphysomes is really the breakthrough part of this technology."
Dr. Irish adds: "I think prostate cancer is an example where these advancements could be very strong and potentially replace surgery down the road if our human trials are successful."
Team effort to get to this point
Theranostics and nanomedicine are rapidly evolving fields of medicine, allowing for simultaneous diagnosis and targeted treatment by pinpointing disease and delivering treatment in a contained and targeted approach.
"Understanding the opportunity to improve patient outcomes across a spectrum of solid tumour cases, this project aims to replace imprecise cytotoxic therapies with nanotechnology-based, image-guided, targeted tumour destruction," says Dr. Stephanie Lheureux, Co-Medical Director of Beyond Chemotherapy at the Princess Margaret.
"With excellent progress made in pre-clinical trials, the team will work towards the first in human porphysomes nanotechnology treatments for cancer surgery patients," adds Dr. John Kuruvilla, Co-Medical Director of Beyond Chemotherapy, "an innovation that aims to improve cancer care through precision and treatment delivery."
Another unique aspect of the trial that Dr. Zheng points to is the team effort it took to get to this point.
"This is a multi-disciplinary collaboration," he says. "The power of this program is that all the disciplines of Princess Margaret have come together, resulting in a sum that is much greater than any one of its parts – the surgeons, medical oncologists, radiation oncologists, radiologists, physicists, chemists, tumor biologists – everything coming together to make progress from the laboratory bench to the patient's bedside."
The Princess Margaret Grand Challenges competition launched in 2020 and is a program that awards bold, innovative and high-impact projects by its clinicians and scientists. The aim is to inspire and advance cancer diagnostics and treatments to cure more patients and improve the quality of life of those living with cancer, focusing on the below pillars:
- Early Detection: detecting cancer early and intercepting it before symptoms, while still curable;
- Beyond Chemotherapy: thinking beyond chemotherapy towards more precise, customized therapies that effectively target cancer to each individual patient, without the harsh side effects of chemotherapy;
- Cancer Digital Intelligence: reimagining and redesigning the cancer patient experience by maximizing digital intelligence and embracing augmented human intelligence;
- The Human Touch in Cancer Care: solidifying the human touch in cancer care by infusing comfort and joy into every interaction, focusing on equity and access, navigation, diversity, ambience of the centre, patient engagement, inclusivity and supportive communication.
Agnico Eagle funds awards for two of the challenges – Early Detection and Beyond Chemotherapy.
To hear more about the pioneering porphysome discovery, listen to Dr. Zheng's episode on the UHN podcast "Behind the Breakthrough".
0 -
I will look into this, thanks. Hope it is available now.0

